Knee injuries
- Mr Damian McClelland, Trauma and Orthopaedic Consultant, and Clinical Director for Musculoskeletal Services at Bupa
- Rachael Mayfield-Blake, Freelance Health Editor
Knee injuries can cause knee pain, swelling, and the feeling that your knee is going to give way (instability). Often it’s the ligaments that are damaged. These are bands of tissue that hold your bones together. You can also hurt other tissues around your knee – for example, cartilage and tendons.
Types of knee injury
Knee ligament injuries
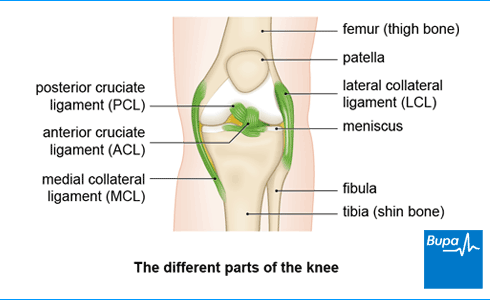
You have two sets of ligaments in your knee. The collateral ligaments and the cruciate ligaments.
Collateral ligament injuries
Your medial collateral ligament (MCL) is on the inner side of your knee and the lateral collateral ligament (LCL) is on the outer side. They limit how much your knee can move from side to side.
- You can sprain or tear your MCL if you get a direct blow to the outside of your knee, which stretches the inner side of your knee. This may happen when you’re skiing, for example.
- You’re less likely to injure your LCL but it can happen if your knee is pushed outwards (away from your other knee). This may happen if you get a blow to the inside of your leg – for example, during contact sports such as football. You can also injure your LCL by twisting on the side of your foot or extending your knee beyond its normal range of movement.
Cruciate ligament injuries
Cruciate means cross-shaped. Your anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL) form a cross inside your knee. They help to keep your knee stable by controlling how much it moves backwards and forwards.
- An ACL injury can be one of the most serious types of knee injury. An ACL injury often happens when you twist your knee – for example, if you land on your leg then quickly turn. This might happen when you’re playing football or basketball, for example.
- Your PCL may get damaged if you fall on your knee while it’s bent. Another way of damaging your PCL is when your knees hit the dashboard during a car accident.
Grading ligament injuries
If one of your knee ligaments is damaged, a doctor may grade your injury to show how bad it is. This will help to work out what treatment you may need and how long your knee injury will take to heal.
- Grade 1 is a stretch of the ligament without tearing it.
- Grade 2 is a partial tear of the ligament.
- Grade 3 is a complete tear through the ligament.
Other soft tissue injuries
Your knee is surrounded by soft tissue that you can damage. Soft tissue means any tissue in your body that isn't bone – for example, cartilage and tendons.
Cartilage injuries
One of the most common knee injuries is a meniscus tear (a meniscus is one of the wedge-shaped pieces of cartilage inside your knee). This can happen if you play a sport that involves twisting – for example, football or basketball. But it can also happen when you run, play tennis, and ski. As you get older, your menisci may become worn, which makes them more likely to tear during normal daily activities.
Your knee also has another type of cartilage called articular cartilage. This covers the ends of your bones inside the joint and it can get damaged too.
Tendon injuries
If you run regularly or play sports where you jump a lot, you may damage the tendons that attach muscles to your knee. You can irritate or tear the tendon that connects your kneecap (patella) to your thigh muscle. This tendon is called the quadriceps tendon. Or you may irritate soft tissue around your kneecap, including the patellar tendon just below your kneecap. This injury is sometimes called jumper’s knee.
Prepatellar bursitis
Housemaid’s knee is the common name for prepatellar bursitis. It’s often caused by the pressure of kneeling forwards for long periods. The bursa (a small fluid-filled sac that acts as a cushion in front of your kneecap) will swell up with fluid. Prepatellar bursitis can also be caused by a direct blow to your knee, by a fall, or by a bacterial infection.
Causes of knee injuries
You may injure your knee if:
- you bang your knee so it moves beyond its usual range of movement – knee injuries can happen from falling or if you land awkwardly
- you play a sport such as football that combines running, jumping, and stopping with quick changes of direction
- you twist your knee, especially in sports such as football or basketball
- your knees hit the dashboard in a car accident – this can damage your posterior cruciate ligament
You’re more likely to have a knee ligament injury if you:
- have knee osteoarthritis because this can weaken the muscles around your knee joint, which increases your risk of injury
- don’t take precautions when you exercise – for example, not warming up before you do anything active or not cooling down afterwards
Symptoms of knee injuries
Knee injury symptoms can vary depending on which part of your knee is affected.
If you have a torn knee ligament, symptoms may include:
- knee pain
- swelling
- instability – you may feel like your knee is giving way
You may also:
- feel or hear a pop or snap at the time you injure your ligament
- find you can't put your full weight on your leg
If you injure a meniscus in your knee, you may:
- have severe pain and your knee may swell after a few hours
- have a ‘locked’ knee that you can’t move in the usual way
- still be able to walk a little on your leg
If you’ve torn your tendons, you may have some knee pain and swelling. You may also find that:
- your kneecap is lying higher or lower than it should be
- you can’t lift your knee
If you have prepatellar bursitis, you may have:
- swelling over the front of your kneecap
- knee pain that’s worse when you bend your knee
- difficulty kneeling and walking
- red skin over your knee
If you have an infection, your knee may look red, and feel hot and painful. You may also have a high temperature. Always see your GP if you have these symptoms.
If you injure your knee and the pain is mild or moderate or has come on gradually, you can visit your GP or a physiotherapist. If your pain is very bad or your knee is badly swollen, go to your nearest A&E department.
Diagnosis of knee injuries
Your doctor or physiotherapist will ask about your symptoms and examine you. They may feel for fluid in your knee joint by pressing gently around your kneecap. They’ll also ask you to describe how you hurt yourself, where your pain is, and what type of pain it is.
Your doctor may ask you to walk, sit, or lie down so they can test for any injury to your knee ligaments or soft tissues. They’ll bend and straighten your knee and move your leg into different positions while diagnosing knee injuries.
If your doctor thinks you need surgery, they’ll refer you an orthopaedic surgeon (a doctor who specialises in bone, tendon, and ligament surgery).
You may need to have some other tests to help diagnose knee injuries.
- An X-ray or CT scan – this can check for a broken bone (fracture) or arthritis.
- An MRI scan – this may help to show up damage to the cartilage or soft tissues of your knee after an injury.
- Knee aspiration – your doctor may remove a sample of fluid from your knee.
- Knee arthroscopy – your surgeon may look inside your knee using a telescope attached to a tiny camera. This can help to show if there’s damage to a meniscus, cartilage, or ligament. Your surgeon may treat your damaged knee at the same time.
Looking for physiotherapy?
You can access a range of treatments on a pay as you go basis, including physiotherapy.
To book or to make an enquiry, call us on 0370 218 6528∧
Self-help for knee injuries
There’s a lot you can do to help yourself if you have a knee injury. It’s a good idea to follow the POLICE procedure.
Protect. Protect your injury from further damage. Rest immediately after the injury but not for long. Consider using some form of support or crutches.
Optimal Loading. Get active sooner rather than later. Start to put weight on your knee and build up your range of movement. Do this gradually – be guided by what feels right for you.
Ice. Place a cold compress such as a bag of ice or frozen peas wrapped in a towel onto your knee. Do this for around 20 minutes every couple of hours for the first two to three days.
Compression. Compress your knee using a bandage to help reduce swelling.
Elevation. Elevate your knee above the level of your heart to reduce swelling. Sit or lie on a chair and use a cushion to raise your leg.
Infographic: POLICE principles
Bupa's POLICE infographic (PDF, 0.5 MB), illustrates the ‘POLICE principles’ to reduce your pain and help you to recover. Click on the POLICE image below to download the PDF.

And there are certain things you should avoid in the first three days after your injury so you don’t damage your knee further. These can be remembered as HARM, which stands for the following.
H – Heat. Don’t have hot baths, showers or saunas, and avoid heat packs and rubs.
A – Alcohol. Drinking alcohol can slow down your recovery and mask your symptoms – increasing the risk that you’ll injure yourself again.
R – Running. Don’t run or do any other form of moderate exercise.
M – Massage. Massaging the affected areas can cause more swelling and damage, so avoid this for the first day or two.
Infographic: HARM principle
Bupa's HARM infographic (PDF, 0.6 MB), illustrates the ‘HARM principle' of things you should avoid doing in the first three days after your injury. Click on the HARM image below to download the PDF.

POLICE and HARM are both are measures you can take to treat any type of soft tissue injury to your knee.
Treatment of knee injuries
Your doctor or physiotherapist may suggest different knee injury treatments, depending on what you’ve done to your knee and how bad the damage is. It’s frustrating, but it’s important to be patient while you recover – your injury may take time to fully repair itself. You may not be able to do all the things you’re used to doing for some time.
Medicines for knee injuries
Over-the-counter painkillers such as paracetamol and ibuprofen can help with the pain if you injure your knee. You can also use anti-inflammatory gels and creams to help with pain relief.
Your doctor may prescribe stronger painkillers that contain codeine if your pain is very bad.
Always read the patient information that comes with your medicine and if you have questions, ask your pharmacist or doctor for advice.
Physiotherapy for knee injuries
If your injury is more severe, or it doesn’t get better over time, your GP may refer you to a physiotherapist. You can also choose to see a physiotherapist privately.
A physiotherapist will create a programme of exercises to gradually strengthen your knee so you can move it normally again. The exact exercises will depend on how you’ve injured yourself, and how badly. But your physiotherapist will probably give you exercises to do every day at home, as well as at your follow-up appointments.
You may need to use a brace to support your knee while it recovers, usually if your injury was severe.
Surgery for knee injuries
Your doctor or physiotherapist may refer you to an orthopaedic surgeon for some knee injuries. You may need surgery to repair the damage to your knee – especially if other treatments haven’t worked.
Your surgeon may suggest you have an operation if you have one of the following injuries and non-surgical treatments haven’t worked.
- You’ve torn your anterior cruciate ligament (ACL), especially if you do a lot of sport or have also a meniscus tear. In ACL reconstruction, your surgeon will take a piece of tendon (usually from your patella tendon or thigh) to replace the damaged ligament.
- Your knee is still painful or locks after an injury to your meniscus. Your surgeon may repair or partially remove your damaged meniscus.
- You’ve injured your medial collateral ligament (MCL) and it hasn’t healed after three months of other treatments. Your surgeon may repair or reconstruct your MCL.
You may be able to have keyhole surgery called a knee arthroscopy to get to the damaged area of your knee.
Prevention of knee injuries
There are several things you can do to reduce your chance of damaging your knee ligaments. These may help to prevent other sports injuries too.
- Exercise regularly to keep your fitness levels up, and include some resistance training (training with weights). Regular exercise will make your muscles stronger and more flexible, so they can support your joints, including your knees. If you haven't been active for a while, start off gently and gradually increase the number, length and intensity of your exercise sessions.
- Warm up before you exercise, and cool down afterwards.
- Wear the right footwear. It’s important that your trainers fit well and you replace them when they wear out. If you’re not sure about the fit, visit a specialist sports shop for advice.
- Wear comfortable clothing that doesn’t restrict you.
- Don’t exercise or play sport when you’re in pain.
- If your occupation involves kneeling or other activity that puts your knees at risk, wear knee pads while you work or kneel on a cushion. This will reduce your chances of getting prepatellar bursitis. And take regular breaks.
How long your knee injury takes to heal depends on which part of your knee you’ve injured and how badly it’s affected. If you play sports or go running too soon, you’re likely to hurt yourself again. So always follow your doctor or physiotherapist’s advice.
For more information, see our section on treatment of knee injuries.
Osteoarthritis can lead to a weakening of the muscles around your knee joint, which increases your risk of injury. If your knee is painful from arthritis, you might not put your full weight on it and you may be more likely to fall over. Regular strengthening and stretching exercises can help reduce your risk of a knee injury.
For more information, see our section on causes of knee injuries.
Common knee injuries include a sprain or tear of your medial collateral ligament (MCL), which is on the inner side of your knee. Or you may injure the lateral collateral ligament (LCL) on the outer side of your knee. Other ligaments you might injure include the anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL), which form a cross inside your knee. You can also damage other soft tissues around your knee – for example, your cartilage and tendons. One of the most common cartilage injuries is a meniscus tear. This can happen if you play sports that involve twisting – for example, football.
For more information, see our section on types of knee injury.
You can tell what kind of knee injury you have by the symptoms you get. If you have a torn knee ligament, you’ll probably have knee pain, swelling, and you may feel like your knee is giving way. And you may feel or hear a pop or snap at the time you injure your ligament. If you’ve torn your tendons, you may find your kneecap is lying higher or lower than it should be. If you have prepatellar bursitis, the pain may be worse when you bend your knee.
For more information, including when to see a doctor, see our section on symptoms of knee injuries.
Three signs of a meniscus tear are:
- severe pain and swelling of your knee after a few hours
- a ‘locked’ knee that you can’t move in the usual way
- that you may still be able to walk a little on your leg
For more information, see our section on symptoms of knee injuries.
Did our Knee injuries information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Knee sprains and meniscal injuries. MSD Manuals. msdmanuals.com, reviewed/revised July 2023
- Assessment of knee injury. BMJ Best Practice. bestpractice.bmj.com, last reviewed 16 September 2023
- Ligament. Encyclopaedia Britannica. www.britannica.com, accessed 16 October 2023
- Knee ligament injuries. Patient. patient.info, last updated 16 August 2022
- Knee soft tissue injury (ACL, LCL, MCL, PCL) management in the ED. Medscape. emedicine.medscape.com, updated 18 August 2021
- Yaras RJ, O'Neill N, Yaish AM. Lateral collateral ligament knee injuries. StatPearls Publishing. www.ncbi.nlm.nih.gov, last update 20 May 2022
- Knee ligament injuries. Patient. patient.info, last updated 16 August 2022
- Meniscal tear. BMJ Best Practice. bestpractice.bmj.com, last reviewed 2 October 2023
- Meniscal tears and other knee cartilage injuries. Patient. patient.info, last updated 16 August 2022
- Knee pain – assessment. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised August 2022
- Pope JD, El Bitar Y, Mabrouk A, et al. Quadriceps tendon rupture. StatPearls Publishing. www.ncbi.nlm.nih.gov, last updated 22 April 2023
- Prepatellar bursitis. Medscape. emedicine.medscape.com, updated 9 January 2023
- Sprains and strains. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised September 2020
- Osteoarthritis. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised October 2022
- Meniscal injury. Medscape. emedicine.medscape.com, updated 19 November 2021
- Personal communication, Mr Damian McClelland, Trauma and Orthopaedic Consultant, 21 November 2023
- Hsu H, Siwiec RM. Patellar tendon rupture. StatPearls Publishing. www.ncbi.nlm.nih.gov, last updated 13 February 2023
- Preparing for a knee arthroscopy. Royal College of Anaesthetists. www.rcoa.ac.uk, published July 2022
- Bezuglov E, Khaitin V, Shoshorina M, et al. Sport-specific rehabilitation, but not PRP injections, might reduce the re-injury rate of muscle injuries in professional soccer players: A retrospective cohort study. J Funct Morphol Kinesiol 2022; 7(4):72. doi: 10.3390/jfmk7040072
- Knee ligament injuries. Patient. patient.info, last edited 10 February 2023
- Medial collateral ligament injury. BMJ Best Practice. bestpractice.bmj.com, last reviewed 16 September 2023
- Find a chartered physiotherapist. Chartered Society of Physiotherapy. www.csp.org.uk, last reviewed 24 January 2023
- Treatment for knee pain. Chartered Society of Physiotherapy. www.csp.org.uk, last reviewed 26 March 2020
- Musculoskeletal problems. Oxford Handbook of General Practice. Oxford Academic. academic.oup.com, published June 2020

